Kansas descended further into the danger zone this week, as evidence mounted that our health care system is
already struggling under the weight of COVID-19, with infections still climbing rapidly. Several of the state's largest hospitals, including
Stormont Vail in Topeka and the
University of Kansas Hospital in KCK, have now suspended elective procedures and put their "surge" plans in place, adding ICU beds for the crush of new patients. But the health care workforce is
already overextended and with record numbers of new infections this week, no matter what we do, it's likely that some people who would have otherwise survived COVID-19 are going to die from lack of timely treatment. But that doesn't mean we shouldn't try to do something. If you're a train conductor and you see that there's another train on the tracks ahead of you, you apply the brake as quickly as you can. Even if you know you won't be able to stop in time to prevent a collision, you want to limit the number of train cars you end up plowing through.
The Good: The infection reproduction rate, or Rt, ticked down ever so slightly last week, from 1.22 to 1.20. That's not enough to prevent catastrophe, given our current rate of new infections. But at least it's trending in the right direction.
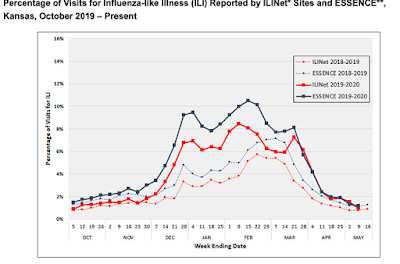
The Bad: ICU availabilty, as reported to KDHE by the federal government, was about 34% as of Nov. 12, or about the same as the week before. But that data seems incomplete, in part because while hospitals may be certified for that many beds, they may not have enough healthy staff for that many beds (health care workers are getting COVID too). The Kansas Hospital Association reported that as of Nov. 13, only 20% of staffed ICU beds were available statewide, and only 10% were available in the KC area. Regardless of which dataset you look at, we're at new record highs for COVID-19 patients in ICU (211 as reported to KDHE and 232 as reported by the hospital association). With more arriving every day. More than 20% of our ICU beds statewide are now taken up by COVID-19 patients, which is daunting considering we often exceed 80% of ICU capacity during flu season, even in non-pandemic years. Please pray for our health care workers, and do everything you can to support them in the coming weeks. Their physical and mental health are going to be severely taxed.
The Ugly: Test positivity in Kansas rose to 58.7% last week according to Johns Hopkins, second-worst in the nation behind South Dakota. That's absurd.
Bonus: Bonus content this week is an open letter to Ron Ryckman, a state representative from Olathe who is the Speaker of the Kansas House of Representatives. His email is ron.ryckman@house.ks.gov if you would like to write him too.
Dear Speaker Ryckman,
Like many Kansans, I read that you were hospitalized for about a week in July because of what must have been a relatively serious case of COVID-19. I was glad to hear that you were discharged with a clean bill of health and hope your recovery has gone smoothly since.
I don't know where you were hospitalized, but based on what I know about our hospitals here in Kansas City, no matter where it was, you probably got excellent care. And though I don't know you well personally, I know you well enough to believe that you sincerely want every Kansan to receive the same level of care. I'm writing to you because, by all accounts, we are approaching a point where that will no longer be possible and you, perhaps more than anyone else in the state, have the power and influence to do something about it.
You are a Republican leader who represents eastern Kansas, has roots in western Kansas, and can speak firsthand to the experience of being hospitalized with COVID. That is unique, and perhaps gives you the ability to convince your colleagues that we must change our current approach or our hospitals will be overwhelmed. (If you have kept in touch with any of the people who treated you in July, please ask them what things are like in their hospital today.)
A statewide mask mandate would be the most obvious thing to do, with the least negative consequences, practically speaking. You probably have heard people say that masks don't work (Lord knows I have). Fortunately, there is much evidence to the contrary. The CDC's mask recommendation is based on 45 different studies.
There's evidence that masks reduce transmission of COVID-19 among people who live in the same state.
There's evidence that masks reduce transmission of COVID-19 among people who live in the same community.
There's evidence that masks reduce transmission of COVID-19 among people who live on the same ship.
There's even evidence that masks reduce transmission of COVID-19 among people who live in the same house.
There's also evidence that mask material reduced transmission of COVID-19 among hamsters in cages who were intentionally exposed to the coronavirus (an experiment that we can't do ethically on humans, but is useful because it stripped away all other possible explanations for the reduction in transmission).
I was heartened to see legislative leaders recently agree to something regarding masks: a $1.5 million allocation to the state hospital association for a public service announcement campaign. But this seems insufficient. By the time the PSA is produced and broadcast, our hospitals may already be full. And it doesn't seem like mask compliance is a matter of public awareness at this point. Most people are aware that health officials recommend wearing masks. Unfortunately there is a partisan divide in attitudes toward masks. A bipartisan mask mandate would send a powerful message that masks are not political, but rather just a tool to help Kansans protect each other.
I'm well aware that pushing for a mask mandate would put you crosswise with some of your colleagues. But I believe the politics of mask mandates is shifting fast as hospitals fill up. In just the last few weeks, very conservative leaders in extremely red states like Iowa, North Dakota, Utah and West Virginia have all enacted new mask requirements.
Several of them also enacted new restrictions on gathering sizes, winter sports, and hours of operation for bars. Based on the epidemiological curve of COVID spread, we're only a few weeks behind those states in terms of hospital strain. No doubt many epidemiologists would recommend we take the same measures as them, and more. But at a minimum, shouldn't we do what has little-to-no negative practical consequences: require masks?
Think back to when you were in the hospital in July, probably on supplemental oxygen, since that is generally the benchmark for when a COVID-19 case requires hospitalization. But this time imagine that instead of being in a room, you're in a bed in a hospital hallway or an overcrowded emergency department. Imagine that even with an oxygen mask on, you start to find it difficult to catch your breath (a terrifying experience I'm unfortunately personally familiar with). Imagine that you're mashing the nurse call light, trying to get someone to help you, but no one comes. You can see medical personnel rushing around, tending to other people who are coding even as you grow more and more lightheaded yourself. But there just aren't enough of them.
This is what we're heading for unless we do something to change our current trajectory.
Sincerely,
Andy Marso